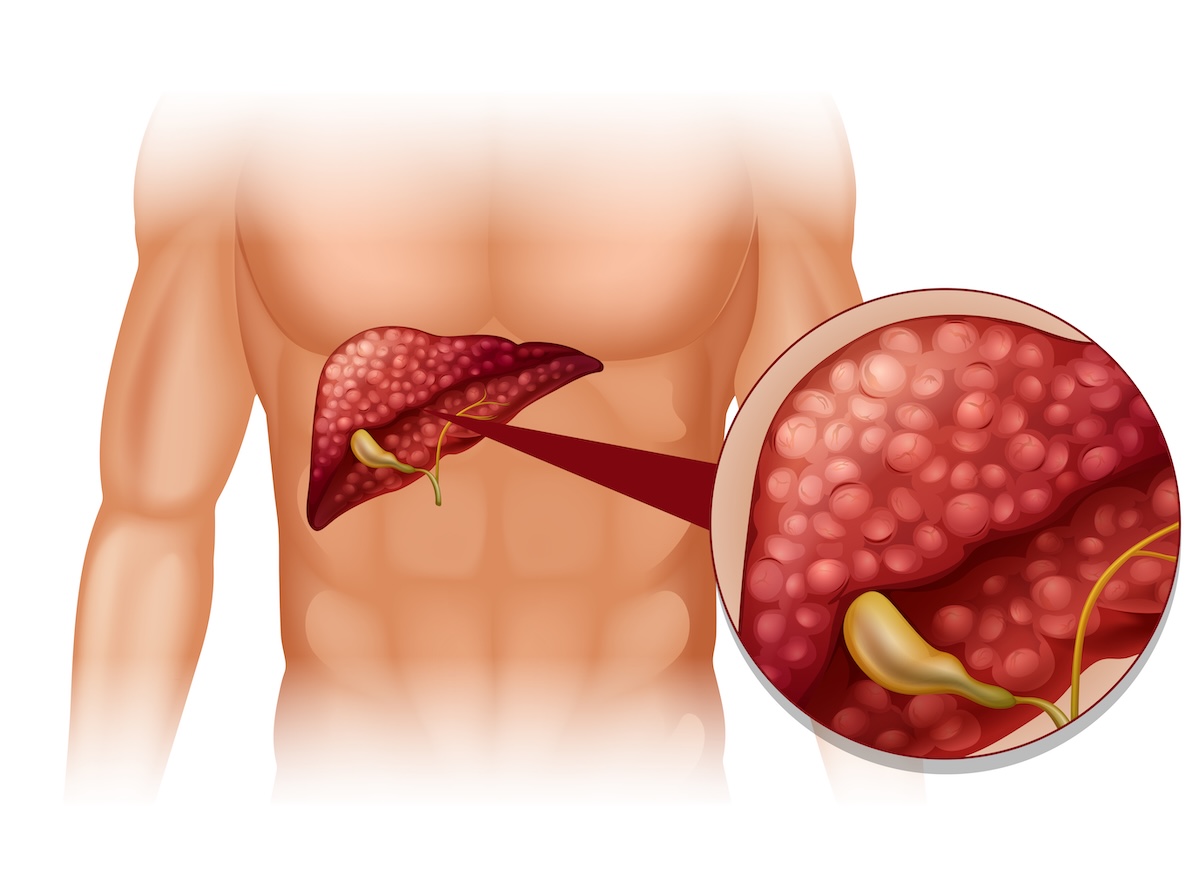
Pancreatic cancer is a serious disease that starts in the pancreas — an organ located behind the stomach. The pancreas helps your body digest food and regulate blood sugar by producing insulin and digestive juices. When cancer develops, abnormal cells begin to grow out of control in the pancreas. Over time, these cancer cells can form a tumor and may spread to nearby tissues or other parts of the body.
This cancer is often difficult to detect early because symptoms usually don’t show up until the disease is more advanced. That’s why it’s important to know the possible warning signs and understand how it is diagnosed and treated.
What Is Pancreatic Cancer?
Pancreatic cancer happens when cells in the pancreas start growing and dividing uncontrollably. In most cases, the cancer begins in the ducts that carry digestive enzymes. This form is called pancreatic ductal adenocarcinoma and is the most common type.
As the cancer grows, it may block the bile duct, affect how the pancreas works, and eventually spread to other organs like the liver or lungs. Because of its location and how fast it can grow, pancreatic cancer is often found late, making it harder to treat.
Causes and Risk Factors
Doctors don’t know exactly why pancreatic cancer develops, but they do know several risk factors that can increase your chances of getting it. One of the biggest is smoking. Smokers are much more likely to develop pancreatic cancer than non-smokers.
Other risk factors include being over age 60, having a family history of pancreatic cancer, having chronic pancreatitis (long-term inflammation of the pancreas), obesity, diabetes, and long-term exposure to certain chemicals. People with inherited gene mutations, such as BRCA2, are also at higher risk.
Types of Pancreatic Cancer
Pancreatic cancer falls into two main categories:
-
Exocrine tumors: These are the most common and start in the cells that produce digestive enzymes. Pancreatic ductal adenocarcinoma is the most frequent type.
-
Neuroendocrine tumors: These are rare and start in the hormone-producing cells of the pancreas. They usually grow more slowly than exocrine tumors and may cause hormone-related symptoms.
Symptoms of Pancreatic Cancer
In the early stages, pancreatic cancer may not cause any symptoms. When symptoms do appear, they may include:
-
Yellowing of the skin and eyes (jaundice)
-
Upper abdominal or back pain
-
Unexplained weight loss
-
Loss of appetite
-
Fatigue
-
Nausea or vomiting
-
Dark-colored urine and pale stools
-
New diagnosis of diabetes or worsening blood sugar control
These symptoms can also be caused by other conditions, but if they persist, it’s important to see a doctor.
How It’s Diagnosed
If your doctor suspects pancreatic cancer, they will start by asking about your symptoms, health history, and risk factors. A physical exam may be done, but the pancreas is deep in the body and not easy to feel. Imaging tests are usually the first step, including CT scans, MRI, or endoscopic ultrasound. These tests allow doctors to see the pancreas and check for tumors.
If a tumor is found, a biopsy is done to confirm the diagnosis. This means a small sample of tissue is taken and checked for cancer cells. Blood tests may also be used to look for certain markers linked to pancreatic cancer.
Once the diagnosis is confirmed, the cancer is staged to see how far it has spread. Staging helps doctors plan the best treatment.
Treatment Options
Treatment for pancreatic cancer depends on the type, location, and stage of the disease, as well as the patient’s overall health. Common treatment options include:
-
Surgery: Used to remove the tumor if the cancer hasn’t spread too far. This may involve removing part or all of the pancreas, and sometimes nearby organs.
-
Chemotherapy: Involves strong medications that kill cancer cells or stop them from growing. It’s often used after surgery or when surgery isn’t an option.
-
Radiation therapy: Uses high-energy rays to kill cancer cells. It may be combined with chemotherapy or used when surgery isn’t possible.
-
Targeted therapy: Uses drugs that focus on specific features of cancer cells to stop their growth. Not all patients are eligible, but testing can show if it’s an option.
-
Immunotherapy: Helps the body’s immune system recognize and attack cancer cells. This treatment may be useful in certain types of pancreatic cancer.
-
Palliative care: Focuses on relieving symptoms and improving quality of life. It can be given alongside other treatments to help manage pain, digestive issues, or fatigue.
Living with Pancreatic Cancer
Being diagnosed with pancreatic cancer can feel overwhelming, but you don’t have to go through it alone. Many people find strength through their care teams, family, and support groups. Depending on the stage and treatment, some people are able to manage their symptoms and maintain a good quality of life.
Healthy habits like eating a balanced diet, staying active when possible, and getting enough rest can help you feel better during treatment. Mental health support is also important, as it can help reduce stress and provide emotional support.

